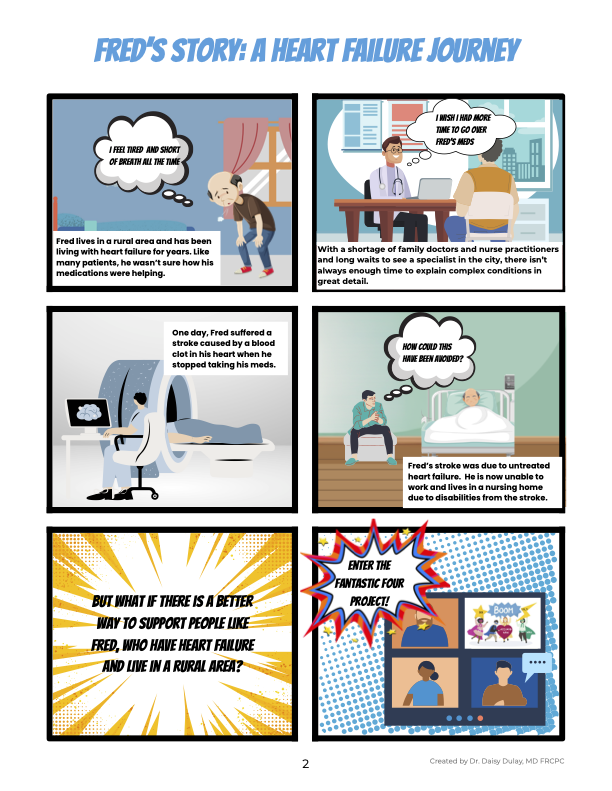
Cardiologist Dr Daisy Dulay and pharmacist Michael Matula joined forces to develop a more effective approach to caring for heart failure patients in rural British Columbia.
Through a quality improvement project funded by the Northern Interior Rural Division of Family Practice and supported by the Northern Interior Rural Primary Care Network (PCN), Dr Dulay and Michael trialed a new care model with seven patients that safely improved their medication management. The model also addressed challenges of accessing health care in rural and remote areas, allowing patients to receive care in their communities without travelling for specialist appointments.
“There are four foundational medicines—the ‘fantastic four’—needed to support people feeling better and to reduce their risk of hospitalization and premature death as a result of heart failure,” says Dr Dulay.
About 750,000 people live with heart failure in Canada, and 100,000 are diagnosed with it each year. It’s one of the top reasons for hospitalizations in Canada, and one in five heart failure patients is readmitted to hospital within one month of discharge.[i]
Determining the most effective dose of each of the four heart failure medications while minimizing side effects for the patient is complex and involves increasing the dosages of each drug, a process called titration.
“As a specialist, I’m not able to see patients fast enough to titrate these medications,” says Dr Dulay. “Leveraging the PCN pharmacist to do that, who checks in with me and follows my titration plan—saves the patient from an appointment with me.”
The new care model brings together the patient, their family physician or nurse practitioner, Dr Dulay, and Michael for hybrid in-person/virtual visits, supported by the Rural Coordination Centre of BC. This allows the patient timely access to the cardiologist without having to travel. Dr Dulay then refers the patient to Michael for ongoing medication management and education support.
Michael has ongoing conversations with each patient about why their drug dosages need to increase. Shifting this work to the pharmacist from family physicians and nurse practitioners frees up their time for appointments with other patients.
“There’s often pushback from patients and families saying, ‘I’m feeling fine, why do I need to increase these meds?’” says Dr Dulay. “Heart failure is not curable in most cases, and we know there’s 50% mortality in five years. We need to find the drug dose that each patient maximally tolerates and then keep them on it, adjusting as things evolve.”
As the patient progresses on their care plan, Michael suggests medication changes to their family physician or nurse practitioner and orders lab work as needed, with Dr Dulay available for consultations and reassessments. When needed, BC Emergency Health Services community paramedics provide home heart monitoring of the patient’s blood pressure, heart rate, and weight.
With this new care model, “we were able to get the patients to their stable dosing of heart failure meds sooner than we would have otherwise,” says Dr Dulay. “Through the assistance of PCN pharmacists, we’ve been able to achieve the maximally tolerated dosages in all four of the medications with the patients participating in this project.”
None of the patients participating in this project experienced any adverse events or required an unexpected ER visit or hospitalization as a result of the medication changes.
Once the patient’s medication is optimized, they transition from the team to maintenance care with their family physician, nurse practitioner, or the heart function clinic if further heart failure management is required.
Errol Winter, Executive Director of the Northern Interior Rural Division of Family Practice, believes they’ve found a way to see patients more quickly, which means patients spend less time in the health system. He believes the new care model provides more effective treatment and better patient outcomes.
“Heart disease is probably the hardest chronic disease to treat in this way [using this care model], and that’s why I chose specifically to do it,” says Dr Dulay. “If we can prove that we can do this with heart failure, then other disease models could be done this way too, like diabetes management, high blood pressure, cholesterol, or COPD [chronic obstructive pulmonary disease].”
Heart failure is caused by various conditions—such as high blood pressure, diabetes, coronary artery disease, and heart attacks—that damage the heart so it doesn’t pump enough oxygenated blood throughout the body. Symptoms include fatigue, swelling in the limbs and abdomen, shortness of breath, coughing and wheezing, weight changes, increased heart rate, and confusion.
Dr Dulay and Michael designed the project to be scalable throughout BC. To spread this work, they’redeveloping a plan to upskill additional pharmacists through the PCN.
Family physicians and nurse practitioners in the Northern Health region or the Northern Interior Rural Division of Family Practice catchment area can participate in this project by contacting Michael Matula at michael.matula@northernhealth.ca or Karen Shepherd, Virtual Medical Office Assistant, Real-Time Virtual Support with the Rural Coordination Centre of BC, at kshepherd@rtvs-bc.ca.
The project was co-led by Dr Daisy Dulay, cardiologist, and Michael Matula, Northern Interior Rural PCN pharmacist. Dr Dulay is a Clinical Assistant Professor in the Department of Medicine at the University of British Columbia, the provincial medical co-lead for SSC’s Spreading Quality Improvement initiative, and RCCbc’s clinical lead for Real Time Virtual Support Consultation to Conversation 2.0 initiative and the Quick Reply Pathway. She is also a member of the Health Data Coalition Board of Directors.
This work took place on the lands of the Nadleh Whut’en, Stellat’en, Ts’il Kaz koh, and Saik’uz First Nations communities in the Burns Lake, Fraser Lake, and Vanderhoof area. The project team recognizes the deep histories, cultures, and contributions of these Nations and is committed to ensuring the work supports equitable, accessible, and people-centred health care for all.
The work was funded by the Northern Interior Rural Division of Family Practice. The Divisions of Family Practice are funded by the Family Practice Services Committee (FPSC).
Partners in this work included participating patients, family doctors and nurse practitioners, Northern Interior Rural PCN, BC Emergency Health Services Home Health Monitoring Program, the NORTH Heart Function Clinic staff and physicians, the Rural Coordination Centre of BC (RCCbc), which is funded by the Joint Standing Committee on Rural Issues, the Specialist Services Committee’s Spreading Quality Improvement and Physician Quality Improvement programs, Northern Health, Interior Health, and the Health Data Coalition.
FPSC is one of four joint collaborative committees (JCCs) that represent a partnership of the provincial government and Doctors of BC. The JCCs also include the Specialist Services Committee (SSC), Shared Care Committee, and the Joint Standing Committee on Rural Issues (JSC).
Read more:
- https://hdcbc.ca/fantastic-four-a-patient-centric-approach-to-heart-failure-management-heart-failure-guideline-directed-medical-therapy-gdmt/
- For the public: https://www.healthlinkbc.ca/healthwise/heart-failure
- For health professionals: https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/heart-failure-chronic
[i] Heart & Stroke Foundation of Canada. https://www.heartandstroke.ca/what-we-do/media-centre/news-releases/heart-failure-in-canada-complex-incurable-and-on-the-rise
