Events
Upcoming Events
2025 JCC Conference
October 6 – 7
Sheraton Vancouver Wall Centre
1000 Burrard St, North Tower, 3rd Floor
Vancouver
Visit the JCC Conference event page for registration and more information.
UPDATE
The FPSC Summit was scheduled to take place on October 6th, as part of the JCC Conference.
After careful consideration, the FPSC has decided to reschedule the FPSC Summit and to host this event virtually in early 2026. This change was made to ensure as many family doctors and partners as possible can participate, regardless of travel limitations, scheduling conflicts, or cost constraints.
Although the FPSC Summit will not be part of the JCC Conference this year, family doctors are invited to attend the JCC Showcase on October 7, which will continue as planned. The organizing committee received hundreds of abstracts and primary care will be well-represented in the program.
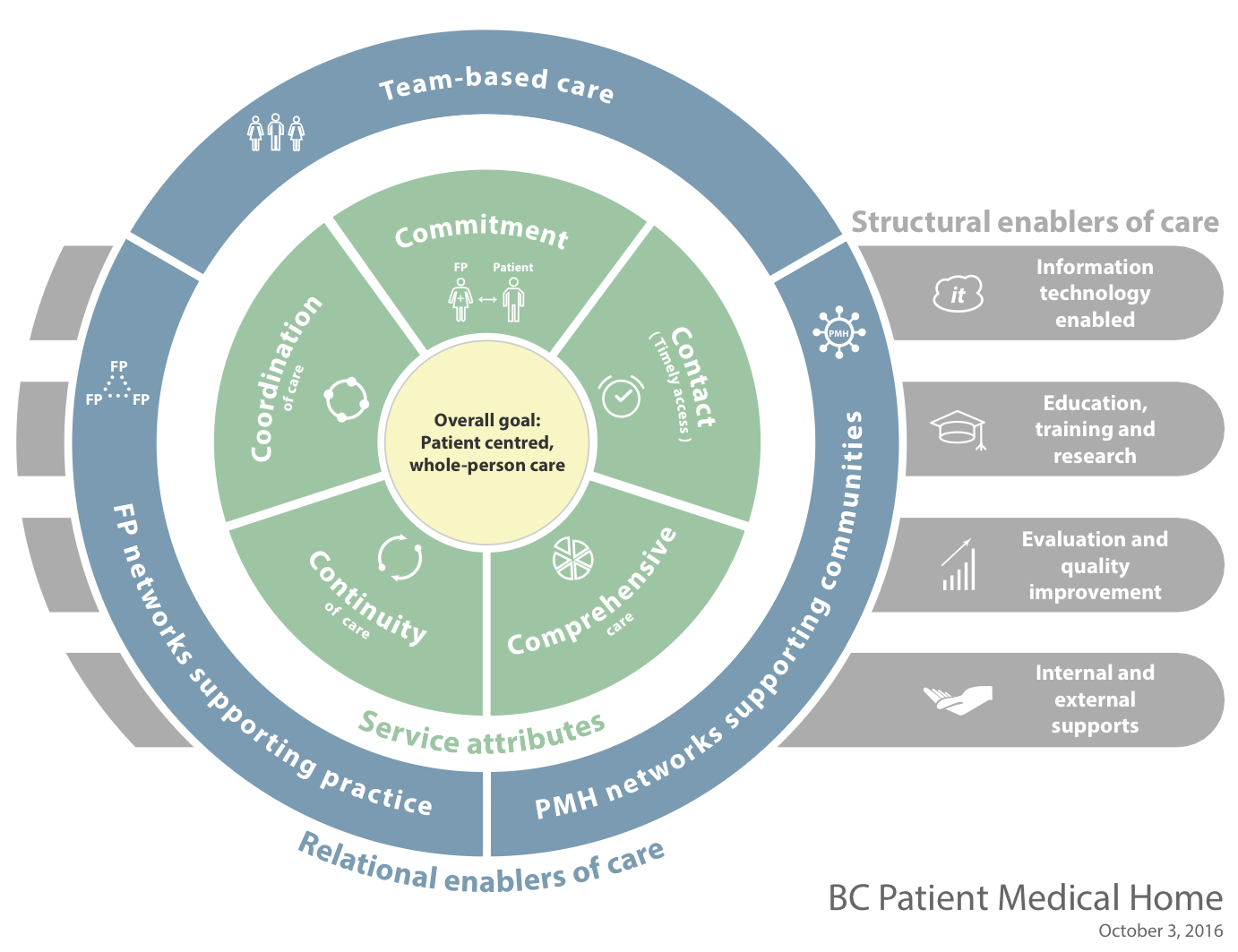
On October 6, 2025, FPSC will hold a strategic planning workshop to discuss FPSC initiatives in the context of a changing primary care landscape in BC. Attendance at this event is by invitation only and will include FPSC Core members, Divisions of Family Practice, key partners organizations, and FPSC staff representation.
In summary, the events are as follows:
- October 6: FPSC strategic planning workshop, by invitation only
- October 6: Specialist Services Committee (SSC) Summit
- October 6 (evening): JCC Conference Reception
- October 7: JCC Showcase (formerly JCC Pre-Forum) featuring presentations from FPSC, SSC, the Shared Care Committee (SCC), and the Joint Standing Committee on Rural Issues (JSC).
- Early 2026: Virtual FPSC Summit, more info to come
2026 FPSC Virtual Summit
Date: To be announced shortly
Past Events
Executive Directors Learning Session and Divisions Learning Session 2025
May 21 – 22, 2025
Coast Coal Harbour Hotel
1180 West Hastings Street
Vancouver
Primary Care Partners Event 2023
October 24, 2023
Physician Leaders and Divisions Learning Event 2022
November 1 – 2, 2022