Panel Management
What is panel management?
Panel management is a process of proactively managing a defined population of patients, using EMR data to identify and respond to patients’ chronic and preventative care needs. The concept is simple: better information about patients leads to better care for patients.
Why do panel management?
The phases of panel management is a framework designed to support doctors as they work to provide longitudinal, proactive care to their patients. An accurate panel means doctors can easily track billings, improve their workflows, improve communications with patients, and maintain a better work-life balance.
The three-phase approach to panel management helps doctors:
- Improve practice workflow efficiencies.
- Identify others who can help family doctors care for their patients.
- Inform and plan proactive care.
What is involved in panel management?
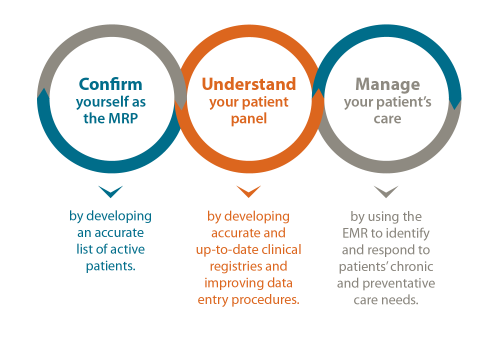
Panel management has three phases:
- Empanelment assigns patients to individual primary care providers. Having an accurate list of active patients for each provider improves continuity of care and enables population-based care.
- Building registries involves creating registries that accurately reflect all patients within the panel that have a specific diagnosis and are properly coded with the correct ICD-9 code.
- Pro-active and preventative care involves using updated data to implement proactive care goals using decision support tools in the EMR.
Compensation
Family practice teams can receive payment for up to 15 hours in total to participate in each phase of panel management. Once three phases have been completed, family doctors will receive a $3,000 bonus payment.
Certification
Family doctors can earn up to 45 certified Mainpro+ credits (three credits per hour), for up to 15 hours in total for the completion of each phase of panel management.
PSP team members can create and support manageable steps to help physicians optimize their EMR data as they work through the phases of panel management.
How do I get started?
Contact your practice support coach or email us at psp@doctorsofbc.ca to get started.
How long does panel management take?
Each phase could take up to 15 hours of physician or staff time to complete and the total time commitment may be up to 12 months. The process is certified for three Mainpro+ credits per hour and is compensated at sessional rates.
Do I qualify for panel management?
To be eligible for sessional compensation, you must:
- Be a Community Longitudinal Family Physician[1] practicing in British Columbia.
- Intend to remain the Most Responsible Physician/Provider (MRP) for your patient panel for at least the next 12 months.
- Be using an EMR system to document and manage patient medical information (including medical history, tests, diagnosis, and treatments) in the clinic you are undertaking panel management.
- Commit to completing phase one, two, and three of panel management in the next 12 months.
Each eligible family doctor can claim payments only once.
For questions about eligibility or payments, contact panel.incentive@doctorsofbc.ca.
Panel management training for medical office staff
GPSC offers medical office staff the opportunity to take the Panel Management for Family Practice program through the University of Fraser Valley. The program consists of seven modules with a final capstone quality improvement project implemented in-practice. It offers practical, skills-based training designed to meet the competencies of a panel manager, including basics of the patient medical home and primary care network, empanelment, registry-based care, pro-active and preventative care.
Current course: Tuesday evenings from January 10 to April 18, 2023.
Deadline to submit applications was December 12, 2022.
[1] A family physician is working as a “Community Longitudinal Family Physician” (CLFP) when they do all of the following:
- Assume the role of Most Responsible Physician/Provider (MRP) for a known panel of patients. The GPSC defines a MRP as a physician who takes responsibility for directing and coordinating the ongoing care and management of a patient. This includes coordinating clinical services delegated to other providers, ensuring cross coverage when MRP is unavailable, and coordinating referrals to specialty care when needed.
- Confirm patient-physician relationship with their patients through a standardized conversation or “compact”, as outlined in PG14070.
- Provide, or coordinate delivery of, longitudinal full scope family medicine primary care services to a patient panel that is inclusive of patients of diverse demographics and medical needs.
- Work in community settings such as physician offices or health care clinics where patients are seen in person. CLFP may also provide some virtual services to their patient panel via telephone, video or other virtual care modality. CLFP may also provide some services to patient panel in facility settings such as hospitals, long term care, hospices, assisted living, or group homes.
- Maintain the comprehensive longitudinal medical records of each patient on patient panel.
A family physician is not considered to be working as a CLFP while they are working solely in one or more of the following health care settings:
- Episodic care settings such as (but not limited to) walk-in clinics, urgent care centres, and hospitals, where physician does not assume the role of MRP for patients.
- Virtual care settings where patient care is delivered via telephone, video, or other virtual care modalities.
- Focused practices serving a specific patient population or providing sub-specialty services such as (but not limited to) maternity care, palliative care, sports medicine, chronic pain, and addiction care.
- Facility settings such as (but not limited to) hospitals, long term care, hospices, assisted living, or group homes.
